ALL is an aggressive type of blood cancer. It is more common in children, though adults are diagnosed as well. The disease develops quickly, sometimes frighteningly fast. We often hear similar stories from patients: “I thought I was just tired, maybe had the flu… and a couple of weeks later I was told it’s leukemia.” That’s why every week, sometimes every day, matters. The diagnosis must be confirmed quickly, and treatment should start without delay.
In Israel, doctors work exactly in this rhythm. They go back over all the tests, clarify the details, and then choose the best therapy — whether it’s standard chemotherapy or innovative medicines. And most importantly, the patient is never left alone: treatment is always accompanied by close monitoring and support.
Confirming the Diagnosis
The first step in Israel is almost always re-checking the diagnosis. Honestly, we often see patients who arrive with a ready report from abroad, and here it turns out the subtype is different. This isn’t bureaucracy — it’s critical. Different ALL subtypes are treated very differently.
What doctors usually do:
- full blood work;
- bone marrow biopsy;
- immunophenotyping — to determine whether it’s a B-cell or T-cell variant;
- molecular testing for mutations and chromosomal changes, including the well-known Philadelphia chromosome (Ph+).
Put simply: doctors break the disease down into details, so they can identify the weak points and attack them with the right therapy.
Treatment Stages in Israel
ALL treatment is always step by step. It’s tough, but thanks to this structured approach survival has improved dramatically in recent years.
- Induction therapy. The very first and most critical phase. The goal is to reach remission — to clear leukemia cells from the blood and bone marrow. Usually this means a mix of chemotherapy and steroids.
- Consolidation. The next step, aimed at destroying the “hidden” cells that remain. This often involves more chemotherapy, and sometimes targeted drugs.
- Maintenance therapy. Less intense, but long-term. Patients may take medicines for months, even years, to keep the disease from coming back.
- Stem cell transplant. Not for everyone. Considered in high-risk cases or if the disease relapses.
Modern and Innovative Approaches
Israeli centers also offer the newest options:
- Targeted therapy. For patients with Ph+ ALL, tyrosine kinase inhibitors (imatinib, dasatinib) are added to treatment.
- Monoclonal antibodies. Drugs like blinatumomab or inotuzumab can directly attack leukemia cells.
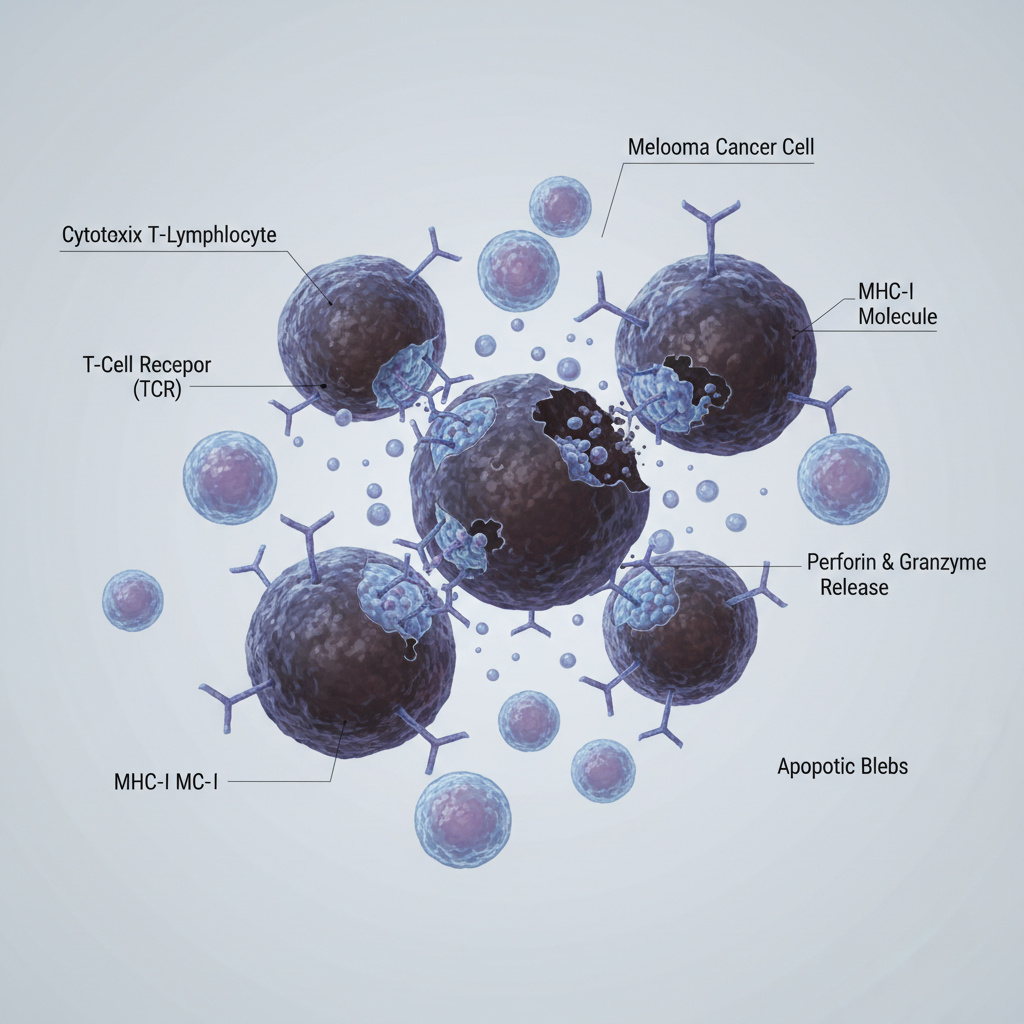
- CAR-T therapy. One of the most advanced methods today. The patient’s own T-cells are modified to recognize and destroy leukemia. In Israel this option is available for relapsed or resistant B-cell ALL and has already changed outcomes for many patients.
- Clinical trials. Some patients join international studies and receive promising new therapies before they become standard.
Patient Support
ALL treatment is intense, so supportive care is critical. This includes blood and platelet transfusions, infection prevention, nutritional support, and psychological help. From our experience, this supportive care often makes the difference — it helps patients, especially children and their families, get through the toughest stages of therapy.
Conclusion
Treating ALL in Israel means more than just standard chemotherapy. For some patients it’s the full multi-step protocol; for others it’s targeted medicines, CAR-T therapy, or enrollment in a clinical trial. What doesn’t change is the approach: care is always individualized. No templates, no “one size fits all.” The plan is tailored to each person, and that’s what gives Israeli centers their strength — flexibility, innovation, and the determination to find solutions even in the most complex cases.





FAQ: Questions Patients Ask About ALL Treatment in Israel
1. Do all patients with ALL need a stem cell transplant?
Prof. Avivit Irit: Not everyone. Some patients do very well with chemotherapy and newer medicines. Transplant is considered mainly for those with high-risk disease or when the leukemia comes back. I always explain to families: it’s not automatic, it depends on the exact case.
2. How do children usually handle the treatment?
Prof. Avivit Irit: Honestly, children surprise us. They adapt better than adults in many cases. Of course, there are tough days — nausea, weakness, infections. But with good supportive care, many kids keep playing, studying, even smiling through treatment. Parents often suffer more emotionally than the children themselves.
3. What happens if the leukemia comes back?
Prof. Avivit Irit: Then we look at new options. Sometimes it’s targeted drugs, sometimes monoclonal antibodies, and yes — in Israel we also use CAR-T therapy. I tell patients: relapse is not the end. It just means we need to change the plan.
4. Are clinical trials safe?
Prof. Avivit Irit: This is a common fear. People hear “trial” and think “experiment.” But in Israel, clinical trials are very strictly controlled. Patients are monitored closely, often more than in routine care. And for some, it’s the only way to access very promising therapies early.
5. How long does the whole treatment usually take?
Prof. Avivit Irit: There is no single answer. The first phase is intense and short, weeks. Then comes consolidation and long maintenance — months, sometimes years. I usually tell families: it’s a marathon, not a sprint. But with every stage, we get closer to long-term control.
6. Can life ever return to normal after ALL?
Prof. Avivit Irit: Yes, many patients go back to school, to work, to family life. It may take time, and there are always check-ups. But I’ve seen children who had ALL grow up, finish the army, start families. That’s what makes this work so meaningful.
For consultation with ALL specialists in Israel:
📞 Phone: +972-73-374-6844
📧 Email: [email protected]
💬 WhatsApp: +972-52-337-3108