Israel is recognized globally for its excellence in hematologic oncology. Patients diagnosed with acute myeloid leukemia (AML) have access to cutting-edge diagnostics, targeted therapies, and advanced bone marrow transplant procedures at Israel’s best hospitals for AML.
Introduction
Acute myeloid leukemia (AML) is a type of blood cancer characterized by an abnormal and increased production of immature white blood cells in the bone marrow, along with a decrease in the number of red blood cells and platelets. This is where the name “leukemia” comes from, which originates from the Greek words meaning “white blood”. Normally, the various types of blood cells are formed in the bone marrow from a small and special group of cells called “hematopoietic stem cells,” which are, as they are called, cells from which all the cells that make up the blood and lymph are formed. Throughout the life of a healthy person, blood and lymph cells are continuously produced from the same small number of stem cells that reside in the bone marrow. Blood and lymph cells multiply and differentiate, acquiring functional abilities that young cells do not have. Indeed, mature red blood cells can carry oxygen and carbon dioxide, platelets activate the clotting system when necessary, and mature white blood cells protect the body from infections.
Acute myeloid leukemia is a cancer of the myeloid cells, which are non-lymphocyte white blood cells that are produced in the bone marrow. It is the most common leukemia in adults. Its incidence increases with age from four people per 100,000 at the age of 40–50 to 15 people per 100,000 in people over the age of 70. AML is characterized by the fact that the population of young cells multiplies uncontrollably and at the same time the maturation and sorting process of the myeloid cell line stops. As a result, on the one hand, the abnormal proliferation of young cells called “blasts” is formed, while at the same time the production of normal blood cells decreases significantly. This process causes the development of anemia with a tendency to bleed and the risk of life-threatening infections.
AML is caused when one of the young cells in the bone marrow undergoes a malfunction in the replication of genetic material, resulting in the formation of an abnormal DNA (Deoxyribonucleic Acid) molecule. The process of leukemia development and the cancerous transformation of a young cell in the bone marrow depend on the nature and number of malfunctions that occur simultaneously, causing the young cell to divide rapidly and not differentiate into mature blood and lymph cells. The time that elapses from the appearance of the initial change to the appearance of the disease itself is unknown. In a minority of cases, leukemia develops from a previous, known disease condition in the bone marrow, such as myelodysplastic syndrome (MDS) or myeloproliferative neoplasm (MPN). Such leukemia is called “secondary” and requires special treatment. Acute myeloid leukemia can also be caused by previous exposure to radiation, chemotherapy, or Prolonged exposure to environmental factors such as benzene (found in tar and asphalt) and various pesticides. However, in most cases, we do not know the cause of the disease.
In most cases, AML has no early signs that indicate that it is about to develop into leukemia. In these cases, the patient feels well right up until the moment the disease is diagnosed in his body. The clinical appearance of the disease is surprising and rapid, and the diagnosis is made following an abnormal blood count result. The symptoms of AML can be different and nonspecific. The most common are infection caused by a lack of mature white blood cells, weakness due to anemia, bleeding from a decrease in platelets or abnormal functioning of the coagulation system, and shortness of breath, which may result from infection, anemia, or the accumulation of many young cells in the small blood vessels of the lungs. Sometimes AML manifests itself acutely, and then the patient needs to be urgent evaluation and treatment by a hematology specialist in Israel to prevent life-threatening complications that can develop even within hours or days.
The Cancer Genome Atlas project has shown that the variety of mutations and genetic changes that occur in a single leukemia cell is very large. In contrast, there are genetic changes that tend to recur with a relatively high frequency in AML patients. The practical clinical significance of a significant number of genetic changes has not yet been sufficiently clarified, but for some of these changes, especially the most common ones, it is possible to describe how they affect the clinical course of the disease and the response to treatment. As a result, a complete and detailed laboratory assessment at the molecular level of leukemia cells is a prerequisite for determining a treatment plan in AML.
AML diagnosis and therapy in Israel
Acute myeloid leukemia is diagnosed by morphological examination when the proportion of blast cells in the bone marrow or peripheral blood is over 20 percent. In order to diagnose the type of leukemia and the stage of arrest of the cells in the myeloid lineage, immunohistochemical staining of the cells and the FACS (Fluorescence Activated Cell Sorter) device are used, in addition to morphological examination. This device is able to identify and characterize the blast cell population based on physical parameters, such as their size and granulation in the cytoplasm, as well as using fluorescently labeled antibodies. These antibodies bind to membrane molecules of hematopoietic cells, which are known as markers that characterize the maturation stages of myeloid cells.
The combination of markers expressed on the surface of the blast cells is partly similar to that expressed in normal myeloid cells and partly abnormal. Leukemia cells are identified by FACS based on their size and motility, and on a combination of markers that are not found on the surface of normally differentiated hematopoietic cells. FACS is a very effective tool in diagnosing and assessing response to treatment, mainly due to its high sensitivity and the short time required to obtain an answer. Another possible use of FACS, taking advantage of the high sensitivity of the test, is to monitor minimal residual disease (MRD) in the bone marrow. While morphological examination using a microscope is not sensitive enough to diagnose a few cells remaining in the blood or bone marrow after treatment, FACS is much more sensitive and is therefore able to detect even a small number of blast cells remaining in the patient’s body. Diagnosis of minimal disease is important because it predicts the possibility of disease recurrence. The use of FACS for MRD monitoring in acute myeloid leukemia has not yet matured into widespread clinical use due to difficulties arising from the heterogeneity of blast cells, which express a phenotype that is not sufficiently specific, and because in many cases the phenotype of the cell population changes between the characterization at diagnosis and the characterization at the time of relapse.
Once the leukemia type is diagnosed as acute myeloid leukemia rather than lymphocytic leukemia, the precise characterization of the leukemia type does not usually affect the determination of the prognosis and treatment of the patient. The prognosis and the probability of a good response to treatment and survival are mainly influenced by factors related to the patient, such as his age, underlying diseases and functional status or by factors related to the way in which the disease developed – whether it is primary or secondary to previous diseases, such as myelodysplastic syndrome, myeloproliferative disease, chemotherapy or appeared without a previously known cause.
In addition, knowledge is accumulating about the importance of specific genetic changes in leukemia cells and their impact on prognosis. The current classification of AML was established in 2008 by the World Health Organization and is based on morphology, cytochemical staining, immunophenotype, clinical syndrome and genetic changes.
Until about a decade ago, genetic changes were diagnosed based on bone marrow karyotype examination alone. Based on these changes, a division into three risk groups was established. The first group included patients with recurrent chromosomal changes, which are unique to acute myeloid leukemia, mainly reciprocal translocations between chromosome segments and the formation of a new fusion protein. Some of these translocations have good prognostic significance, such as the translocation involving the transcription factor Core binding factor, or the (15;17)t translocation characteristic of acute promyelocytic leukemia (APL).
Cytogenetics can be tested with newer laboratory methods. The combined gene resulting from the chromosome translocation can be tested at the DNA level using FISH (Fluorescence in Situ Hybridization) and Reverse Transcription PCR (RT-PCR) analysis. With the help of these laboratory methods, which are more sensitive than karyotyping, peripheral blood cells can also be tested and are also important in monitoring MRD after the patient’s treatment.
The second group is a relatively large intermediate group, which includes 40–50 percent of all patients, in whom the karyotyping test is normal and the prognostic forecast obtained from it is unclear. Following genome mapping, it was discovered that common somatic mutations of prognostic importance can also be found in various genes in these patients. Some of the mutations in genes such as FLT3, NPM1 and C/EBP are tested in a routine test and classified according to the recommendations of the European Leukemia Association.
Additional mutations in the ASXL1 genes, RUNX1 and p53 have been shown to be associated with poor prognosis. Some of the other mutations have triggered the development of drugs targeting the protein carrying the mutation. Indeed, some of them, such as an IDH1 inhibitor, are in advanced stages of research and are expected to bring hope to AML patients carrying the specific mutation. The complexity of mutation testing is great because of the presence of several different somatic mutations in a patient. Some of these mutations involve only a portion of the leukemia cells, and it is not always possible to assess the clinical significance of the presence of a particular mutation in only a tiny subpopulation of cells. Furthermore, the composition of mutations in leukemia sometimes changes during the course of the disease, making it difficult to follow the development of the disease.
The third group includes patients with chromosomal changes that predict an extremely poor prognosis, such as a complex karyotype with more than three changes, or the absence of a chromosome or part of it.
Initial Treatment for Acute Myeloid Leukemia
AML treatment in Israel consists of two phases. The first part is called the “induction phase,” and it is an intensive effort to eliminate the malignant cells from the blood and bone marrow. The success of induction is measured by reaching a state called “Complete Remission,” which is characterized by the patient’s blood count returning to normal and no disease cells can be clearly seen on a bone marrow examination.
Advanced leukemia care in Tel Aviv
The most effective treatment available for the induction phase is chemotherapy based on a combination of at least two chemical drugs – cytarabine and daunorubicin (Cerubidine) – which are administered simultaneously intravenously for seven days. Remission induction treatment leads to a dramatic decrease in blood counts and a serious risk of life-threatening infections and bleeding. Therefore, it is preferable that this treatment be given in a hospital under conditions of observation and isolation.
Achieving a complete remission is essential, and therefore, if necessary, double induction therapy is given by an additional round of chemotherapy shortly after the first treatment. In some European countries (mainly Germany and England), it is customary to give all patients with acute myeloid leukemia two consecutive rounds of chemotherapy in order to increase the chance of achieving a complete remission. In the rest of the world, including the United States and Israel, it is customary to perform an assessment in the days following the initial chemotherapy, and based on this, decide whether to give an additional round of induction therapy. This assessment is combined: on the one hand, the patient’s general condition and the risk that would be added if he were given an additional round of chemotherapy are assessed; on the other hand, the degree of response in the bone marrow is assessed by a repeat bone marrow examination performed 12–14 days after the start of the first induction round. The success rates and risks of induction therapy for AML depend mainly on the patient’s age and general condition, but also on the specific molecular parameters of the disease.
In general, the rate of entering remission decreases from about 75 percent in young people to about 50 percent in adults over the age of 60, and mortality rates from complications (mainly infectious) increase from about 4 percent in young people to about 8–10 percent in adults over the age of 60.
Complementary therapy after achieving remission
The main problem in the treatment of acute myeloid leukemia is the high recurrence rates of the disease. Complete remission is a state in which the normal bone marrow has recovered at the end of chemotherapy and no leukemia cells can be clearly seen on examination, but it does not mean a complete cure. In order to try to achieve a complete cure, additional treatment is necessary, and the choice of the type of additional treatment depends on the patient’s and the disease’s data.
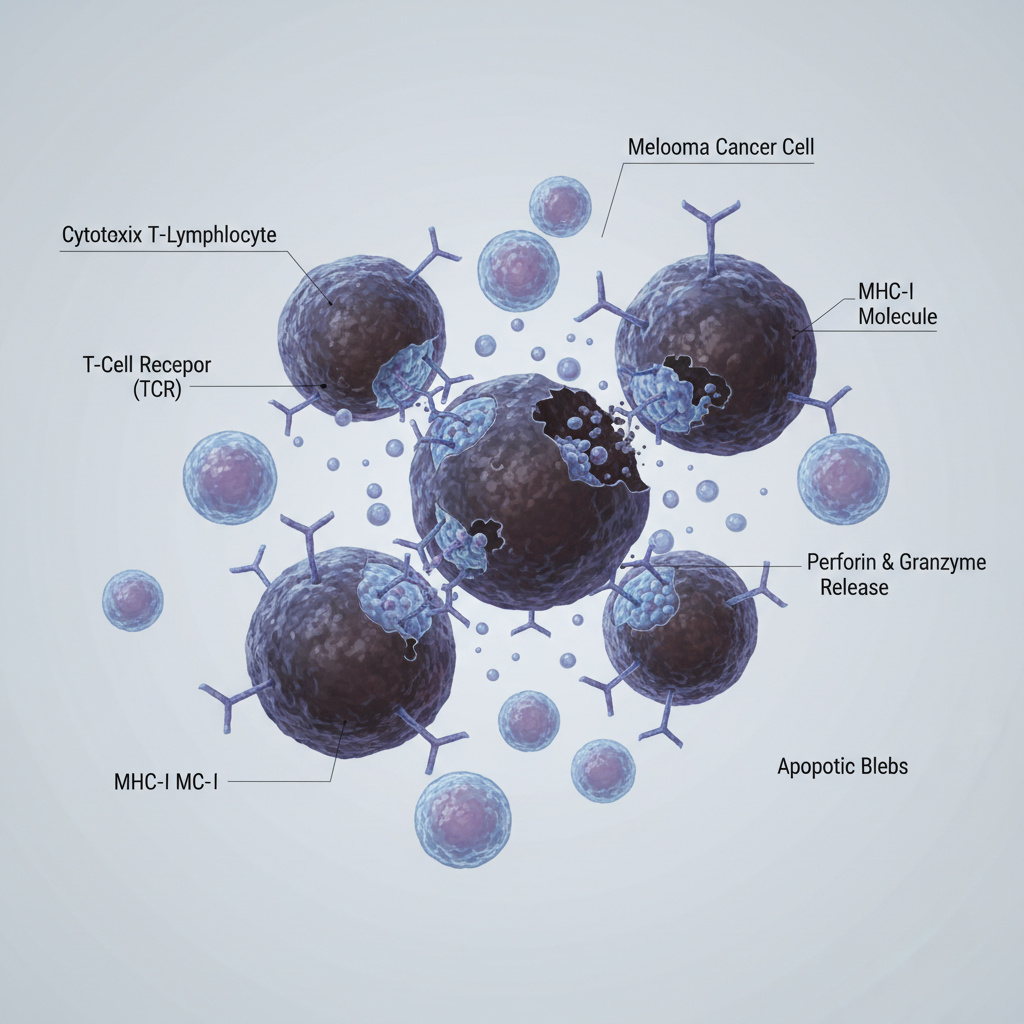
The types of treatments given after achieving remission can be divided into two main groups. When the patient’s general condition is good and our intention is to achieve a complete cure, the degree of risk of disease recurrence, determined based on the molecular profile of the disease, affects the choice of complementary treatment. In cases where there is a high risk of disease recurrence, it is assumed that there is a reasonable chance that the patient’s body contains, even in a state of complete remission, a remnant of disease cells that are resistant to chemotherapy. Therefore, the medical recommendation is to proceed to a bone marrow transplant from a matched donor in a specialized Israeli center. The advantage of bone marrow transplantation is that the donor’s immune system is expected to be able to eliminate the remaining disease cells in the patient’s body in an immune-dependent manner that is not affected by the cells’ resistance to chemotherapy.
In cases where the risk of disease recurrence (calculated given the molecular parameters) is lower, the risk of transplantation, which depends on the patient’s age, general condition, and donor suitability, is weighed against the risk of disease recurrence. If the risk of bone marrow transplantation is higher than the risk of disease recurrence, the patient is offered 2–4 more cycles of chemotherapy to eliminate any remaining disease cells that survived induction therapy.
Treatment of AML in Elderly Patients
The incidence of acute myeloid leukemia increases with age, and in addition, older people have more difficulty than younger patients in tolerating intensive chemotherapy. In the past, it was customary to believe that after a certain age there was no place for full treatment in curing older patients, but the approach to this problem is undergoing a revolution. Over time, we have learned that there is a very high variability and significant differences between older people and that the ability to cope with complicated and difficult treatments does not depend on chronological age but on the person’s general health. Many studies have shown that intensive chemotherapy in people over the age of 70 whose general health is good at the time of diagnosis of leukemia can prolong their lives. However, the success rate of treatment in people of this age is decreasing. A statistical fact, the biological basis of which has not yet been clarified, is that the proportion of older patients whose disease is resistant to chemotherapy is much higher than in younger patients. Furthermore, even when remission is achieved in older patients, it is on average shorter than the duration of remission in younger patients. For older patients, for whom a general health assessment has been made and it has been decided not to treat them with intensive treatment, there is no approved registered drug in Israel, included in the drug basket, that could be a good substitute for intensive chemotherapy. In older patients, the rate of disease progression is usually slower than in younger patients, and in Europe, treatment with the drug Vizada (Azactidin), which has been found effective in MDS and leukemia with a low number of blasts in the bone marrow, is approved for them.
The use of new genome sequencing techniques (Next Generation Sequencing) (NGS) in research has led to an understanding of the spectrum and frequency of mutations in AML patients. In most patients, subpopulations of cells characterized by different mutations have been found. The “dominant” cell population changes during the course of the disease, mainly after treatments. The dynamic evolution of different cell populations that occurs during disease relapse likely contributes to resistance to treatments. At this stage, NGS is primarily used as a research tool, but it is of great importance in the era of developing therapies targeting specific mutations.





Summary
For years, many studies have indicated that the development of AML originates from hematopoietic stem cells, their “homing” in bone marrow niches and their migration into peripheral blood, by mechanisms similar to normal stem cells. Leukemic stem cells differ from other leukemia cells in their slow proliferation rate and self-renewal. This difference may explain their resistance to chemotherapy. Common mutations in AML that are involved in epigenetic regulation have been found in progenitor cells before leukemia develops. This important finding supports the theory that in order to eradicate AML and prevent relapse after chemotherapy, targeted therapy of leukemic stem cells is necessary.
For consultation with AML specialists in Israel:
📞 Phone: +972-73-374-6844
📧 Email: [email protected]
💬 WhatsApp: +972-52-337-3108