Neuroblastoma Treatment for Children in Israel
Neuroblastoma is a malignant tumor that develops from cells of the sympathetic nervous system. Most often, it starts in the adrenal glands. But it can also show up in the chest, the abdomen, along the spine, even in the neck or pelvis. The disease usually affects young children, often under the age of five.
Sometimes, this tumor behaves in unexpected ways. In rare cases, it may shrink on its own or transform into a benign tumor. But in most situations, it grows aggressively and spreads quickly — which means families need answers and treatment without delay.
Why does it happen?
This is one of the first questions parents ask us. And the truth is, there isn’t one clear reason. Doctors talk about random genetic mutations, about changes that occur during fetal development. Occasionally, there’s a hereditary component. But for the majority of families, nothing in their lifestyle or choices caused this. It’s not anyone’s fault.
Signs that should alert parents
Symptoms depend on where the tumor is located.
If it’s in the abdomen — the child may complain of pain, the belly may look larger, there could be constipation or trouble urinating.
If it’s in the chest — cough, shortness of breath, swelling of the face and neck, even difficulty swallowing.
If it has spread — bone pain, bruises or dark circles under the eyes, bulging eyes, limping.
The hardest part is that these signs can look like much milder childhood conditions. That’s why parents shouldn’t wait too long before checking.
Diagnosis in Israel: how fast is it really?
The waiting is usually what parents fear most. In Israel, we move quickly. In fact, a full diagnostic process often takes no longer than 3–5 days.
- On the first day, a pediatric oncologist meets the child and reviews all the medical records and scans.
- On the second, tests are done — blood work, imaging like MRI or PET-CT, sometimes biopsy or bone marrow aspiration.
- By the third day, the case is reviewed by a team — oncologist, surgeon, radiologist, geneticist. And by the end of that week, the family already knows the diagnosis and the plan. Parents often tell us: “We never thought it would happen this fast.”
How treatment is usually planned
The approach depends on the stage and the child’s risk group.
At low risk, sometimes careful monitoring is enough. Yes, in some infants, the tumor may regress naturally.
At intermediate or high risk, chemotherapy usually comes first, followed by surgery to remove the tumor. For very high risk cases, treatment becomes more intensive — high-dose chemotherapy, stem cell transplant.
Radiation therapy is also used, but always with the most advanced equipment, and, when needed, proton therapy. It’s safer for children because it spares more of the healthy tissue.
What new treatments are available in Israel?
Parents are often surprised at how many innovative options exist today.
- Targeted therapy — drugs that act on specific tumor mutations.
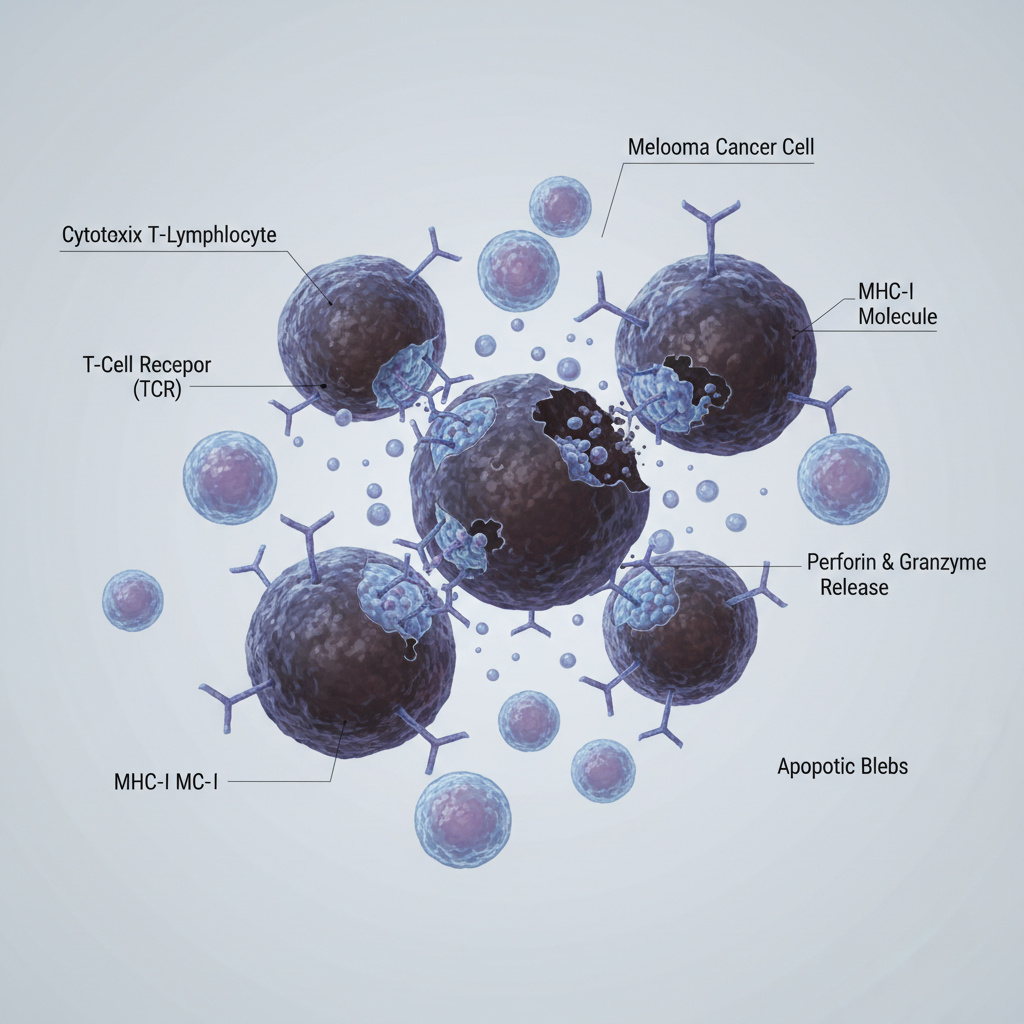
- Immunotherapy — antibodies, vaccines, and sometimes oncolytic viruses that help the child’s own immune system attack the tumor.
- CAR-T therapy — where immune cells are modified in a lab, then reinfused so they can recognize and destroy cancer cells.
- Stem cell transplantation — sometimes even done twice, if the case is very aggressive.
- Proton therapy — a more precise type of radiation that helps protect developing organs.
What about prognosis?
It depends. For children with early-stage, low-risk disease, the chances of cure are very high. Over 90% in some cases. At advanced stages, things are more complex. But here in Israel, we have access to clinical trials, to therapies not yet available in many other countries. That often means we can give families options when they thought there were none left.
Life after treatment
We always tell parents: the treatment itself is just one part of the journey. After therapy, children need careful follow-up. That may include physiotherapy, speech therapy, psychological support. And parents need support too. We try to make sure the family is never alone in this — because recovery is not just medical, it’s emotional and social as well.
Summary
Neuroblastoma treatment in Israel combines advanced technology, rapid diagnosis, and compassionate care for families. Diagnosis is confirmed within days, therapy begins without delay, and children gain access to cutting-edge therapies often unavailable elsewhere.
To consult with specialists in neuroblastoma treatment in Israel:
📞 Phone: +972-73-374-6844
📧 Email: [email protected]
💬 WhatsApp: +972-52-337-3108












FAQ — answers from our Pediatric Hemato-Oncology team
Can neuroblastoma be completely cured in Israel?
Honestly, it depends. At early stages, yes — chances are excellent, and many children fully recover. In difficult cases, treatment is longer and tougher: stem cell transplant, immunotherapy, innovative drugs. But we use every possible option, even when other clinics say “there’s nothing left to do.”
How long does it take to complete diagnostics and start treatment?
Not months — usually just a few days. Three to five on average. Parents are often surprised: “We didn’t expect it to move this fast.” We know the hardest thing is waiting, so we move quickly.
How is treatment in Israel different from other countries?
Mainly the speed of access to innovations. Immunotherapy, CAR-T, proton therapy — they are already part of our practice. And another difference: decisions are not made by one doctor alone. Every case is discussed by a team of specialists.
Is it possible to get an online consultation before traveling?
Yes. Families often send us scans and reports, we review the case and provide a preliminary opinion online. It does not replace an in-person exam, but it helps families prepare and know what to expect.
What is the cost of neuroblastoma treatment in Israel?
Almost every family asks this. And they are right to. There is no universal price: it depends on stage, chosen protocol, and sometimes participation in research programs. We never give “average numbers.” We review the documents first and then provide an estimate.